Infertility is defined as the inability to achieve a pregnancy after 12 months of unprotected intercourse. According to a recent report published by the World Health Organization (WHO), many people experience infertility at some point in their lives. In fact, about 17.5% of adults (that is, about one in six) have this problem. This is why it is urgent to increase access to information and attention to infertility, accessibly and qualitatively, for those who need it.
The male contribution to the infertility of the couple ranges between 30 and 40% of the cases. One in 20 males generally has some type of fertility problem, with low sperm counts in the ejaculate. However, only one in 100 men does not have sperm in his ejaculate. What are the main causes of this? How many have a solution? What to do to avoid it? We will be talking about these issues in the article.
Life of a sperm
Before fully talking about the subject of male infertility, we must refer to spermatogenesis. Or, to put it simply, to the process of formation of the spermatozoa, which are the male gametes. This process occurs in the testicles, specifically in a structure called the testicular seminiferous tubules, and lasts approximately 62 to 75 days.
However, the formation of spermatozoa begins, strictly speaking, much earlier: around day 24 of the embryonic development of the male organism. At that time about 100 germinal cells are produced that migrate towards the buds of the genital organs. About the fourth week of development, they will have become about 4,000.
But it is not until puberty that the testicles begin to produce sperm. This process will continue throughout the life of the man, although the quality and quantity of the spermatozoa may decrease over time.
On the other hand, it is essential to understand that this is a hormonally controlled process. It involves the hypothalamic-pituitary-gonadal axis. Alterations in the secretion of hormones can lead to non-generation of spermatozoa.
Phases of spermatogenesis
Spermatogenesis consists of three phases. In the first, first-level germinal cells are formed from a stem cell, which have a complete set of chromosomes. That is 23 pairs.
In the second phase, the genetic information is halved. In this way, the initial spermatocyte, with 46 chromosomes, divides into two second-level spermatocytes that, in turn, divide into two cells with 23 chromosomes.
The final maturation of the cells occurs in the third phase. During the process, the tail increases in size and the head, which contains the genetic information, decreases and becomes pointed in order to pass through the area that precedes the ovule.
The hormones involved in sperm formation are:
- Testosterone: is responsible for activating the genes that promote the division of germinal cells.
- FSH (Follicle Stimulating Hormone): nourishes the sperm and favors its maturation
- LH (Luteinizing Hormone): activates the release of testosterone.
- Inhibin: inhibits the release of FSH, stopping the process of spermatogenesis.
- Thyroid hormones. they participate in the regulation of the whole process.
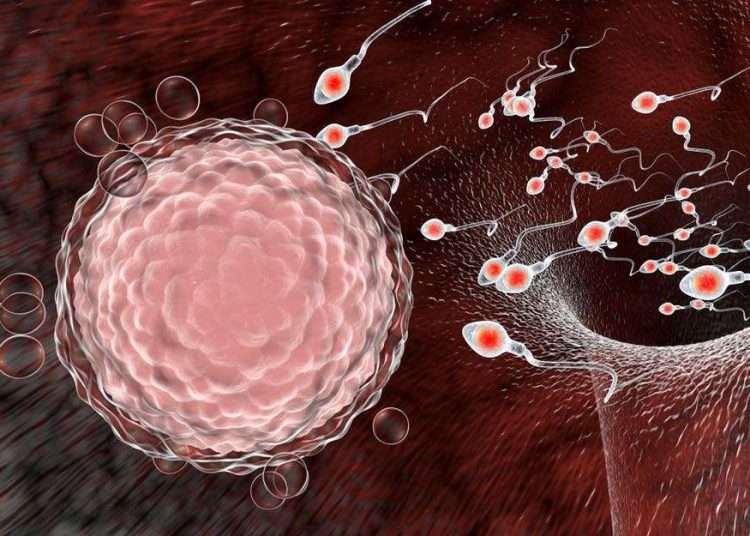
Fertilization: the fascinating path of the spermatozoon to the ovule
The path that the spermatozoon travels to the ovum is divided into two stages, the first occurs within the male sexual organs. The second occurs once the sperm enters the female reproductive system until it reaches the egg and fertilizes it.
During the first stage, about 250 million spermatozoa are covered with seminal fluids from the vesicles of the same name and from the prostate. These fluids preserve their activity and their fertilizing capacity for up to 48 hours after being expelled. If they are inside the female genital apparatus, this vitality can be extended to 72 hours.
The number of spermatozoa per ejaculation depends on several factors such as age, degree of arousal, size of the testicles and frequency of ejaculation. For a man to be considered to have normal sperm (normozoospermia), he would have to have at least 15 million sperm per milliliter of ejaculation or 39 million in the total volume of the sample.
Once the egg is released, the journey becomes a real obstacle course in which the sperm must reach the finish line within 24 hours if it wants to be fertilized, since this is the average life of an egg. For that, it has the propulsive action of the tail, which makes it move.
Among the obstacles that must be overcome is the acid pH of the vagina and the opposition of the white blood cells (defensive cells) that detect the sperm as an enemy cell and try to destroy it. Then, it reaches the utero-tubal junction, the narrowest of the route, and where many spermatozoa are lost. Those who manage to reach the tubes must get around the walls, which exert a force in which many remain attached.
The few that manage to escape must cross the biggest barrier of the entire journey: the zona pellucida of the ovum. It is a layer that surrounds the oocyte. Normally, only one sperm will be able to pass through it.
If the egg has not been released at the exact moment to welcome the sperm — and we have already seen in previous articles that many things can happen so that this does not happen — the whole race will be in vain. The gamete that overcomes all these barriers will be the “winning sperm,” the one that will fertilize the egg.
Types of male sterility
Next, we will see the factors or causes of male infertility. For study, these factors are divided into four groups. However, in a patient, several may coincide and others that we will see later.
- Pretesticular or endocrine factor
This type of sterility is due to problems in the hormonal regulation of spermatogenesis, that is, the production of sperm. The hormones secreted by the pituitary gland (LH and FSH), responsible for acting on the male reproductive function, can be altered for various reasons. Among them:
- Unhealthy lifestyle habits.
- Hypothyroidism and hyperthyroidism.
- Hypogonadotropic hypogonadism.
These alterations may be from birth problems or be caused by external factors, such as some substances or drugs, which can alter the entire hormonal regulation system and cause fertility problems.
- Testicular factor
When speaking of a “testicular factor” reference is made to any alteration or defect that directly affects the testicles. Male infertility due to a testicular cause may have occurred from birth or by external agents at any time in life.
Among the congenital factors are genetic alterations that affect the number of chromosomes or other alterations in gene activity, such as Noonan syndrome.
Among the acquired testicular defects, we will find those produced by drugs, such as those used in the treatment of cancer, drug use, radiotherapy, trauma, infections, etc. The best-known pathologies are varicocele, cryptorchidism, also known as an undescended testicle, orchitis, which is inflammation of the testicles, and testicular hydrocele.
- Post-testicular factor
Male sterility due to post-testicular factors encompasses all those cases that are due to obstructions or alterations in the seminal tract. These are structures that the spermatozoa must cross to come out, once they have been produced.
Among the causes of this obstruction, we can mention infections, particularly those of sexual transmission, traumatisms, the presence of anti-sperm antibodies, among others.
- Sperm factor
Finally, the sperm factor is the most common among the causes of male sterility. This category includes sperm alterations that directly affect their shape, mobility, vitality, or quantity.
To analyze semen quality, a study called a seminogram or spermogram is performed, which makes it possible to diagnose the following alterations:
- Oligozoospermia: Low concentration of sperm in the sample.
- Asthenozoopermin: Alterations in sperm motility.
- Teratozoospermia: High amount of sperm with an abnormal structure.
- Necrospermia: high amount of dead sperm.
- Azoospermia: absence of sperm in the ejaculation.
Opinion of the expert
OnCuba had the opportunity to talk about male fertility with Dr. Iván Donchev Martínez, a specialist in MGI and Urology, who works as a urologist at the Provincial Center for Assisted Reproduction in Humans, in Holguín. Below are the questions we addressed to the expert with his answers.
What is the difference between infertility and sterility?
Infertility is the inability of the couple to carry a pregnancy to term. Sterility, for its part, is the inability to conceive a pregnancy after one year of complete sexual intercourse (with ejaculation inside the vagina) and without the use of contraceptive methods.
What are, according to your experience, the most frequent causes of male infertility in Cuba?
In our environment, sexually transmitted infections that show up in the spermogram as leukospermia are very frequent. That is, the presence of white blood cells or leukocytes, which are the defensive cells of the body, in the sperm. This results in alterations in the concentration, mobility and shape of the spermatozoa and, of course, makes it difficult to achieve a pregnancy. All other causes that have been listed throughout the article are also noted, both genetic and hormonal, diseases such as cystic fibrosis, iatrogenic causes, specifically, afferent duct ligation in varicocele surgery, patients undergoing radiation…
Is there a population group more affected than another?
Among the most affected population groups, I could mention those men who, due to their work, are directly exposed to radiation, electromagnetic waves, or those in direct contact with pesticides.
The genetic component is also fundamental. There are families where sterility in men is very frequent. In these cases, the solution is usually very complicated. In fact, some do not qualify for assisted reproductive techniques and need a donor.
What risk factors for male sterility are common in our environment?
Smoking, inadequate intake of alcoholic beverages, nutritional disorders, sustained psychosocial stress… A good quality of life is essential for satisfactory reproduction, with healthy habits that include frequent physical exercise, adequate sleep schedules, and, even, an intra-family environment that favors conception. Another factor is drug intake, this includes medications and, above all, illegal drugs. The latter is directly related to sterility.
Is it common to face prejudice among patients with any cause of male infertility in our country?
In Cuba, there are many taboos regarding male sterility. Some patients have a hard time accepting it; others simply do not. That’s why, when it comes to fertility, we work with a multidisciplinary team that includes specialists from various branches of medicine, including psychologists.
When should we suspect that we have an infertility problem and what should we do?
We should suspect sterility problems when after a year of complete sexual intercourse, without the use of any contraceptive method, a pregnancy is not achieved. In these cases, the first thing to do is go to the family doctor, who has the mechanisms to refer the patient to the municipal infertility clinic. There the patient will be studied and a treatment will be recommended. If the results are not favorable, he can be referred to the provincial consultation or to the corresponding territorial center.
Are most causes of male infertility curable?
Yes, most causes of infertility are curable or at least manageable and the reproductive health of patients can be greatly improved. Sometimes only with lifestyle modifications, physical exercise, healthy eating, and the reduction of psychosocial stress, patients improve. The use of vitamins, zinc sulfate is also indicated, and in the case of infection in the seminal tract, the use of antibiotics is indicated… Only in a small percentage of cases, the cause cannot be resolved. But, I insist, the majority are treatable and with perseverance and adherence to the indicated treatments, very good results are obtained.
Male infertility: what you should remember
- One in 20 men has some type of fertility problem.
- Spermatogenesis is the process of formation of spermatozoa. It occurs in the testicles but is regulated, among others, by hormones of the hypothalamus-pituitary-gonadal axis.
- For fertilization to take place millions of spermatozoa must be ejaculated. They will face numerous obstacles. Only one will reach the finish line and it will be “the winning sperm.”
- The causes of male infertility are divided into four large groups:
- Pretesticular or hormonal factor.
- Testicular factor.
- Post-testicular factor.
- Sperm factor
- Sexually transmitted infections are one of the most frequent causes of infertility in men in Cuba.
- Those men exposed by their work to radiation, electromagnetic waves, or pesticides have an increased risk of infertility. The genetic component in many cases is decisive.
- Among the fundamental risk factors for male infertility/sterility are the consumption of alcohol, tobacco, sustained stress, poor nutritional habits, sedentary lifestyle.
- If you suspect that you may be suffering from infertility/sterility, you should see your family doctor.
- Most causes of infertility/sterility are curable or at least manageable.